April Showers bring Thunderstorm Anxiety!
Does this scenario sound familiar: The weather channel is calling for sunny skies all day long, but the dog is hiding behind the toilet, shaking, drooling, and refusing to be comforted. Within an hour the sky darkens, the smell of rain is in the air, the first big drops of rain start to plop on the roof, and in the distance you hear that first peal of thunder.
Have you ever wondered if your dog is better at predicting a thunderstorm than the guy on the weather channel? Thunderstorm anxiety is a very common behavioral problem of dogs. They feel the pressure change, they hear those peals of thunder, and then they become inconsolable.
It’s so hard to watch your dog friends feel so much fear and anxiety! We want to just explain to them why being afraid isn’t necessary! Let’s talk about thunderstorm anxiety and noise phobia, and how we can help our canine housemates feel more comfortable.
Thunderstorm anxiety is just a more complicated form of noise phobia. The root of the fear is the noise phobia, but on top of that the dogs often really do feel the pressure changes, changes in wind, and changes in environment that signal an impending storm. Because they are so very aware of their environments, the fear actually starts long before that first boom!
Here’s the core to addressing noise phobia: Don’t over comfort. I know. It’s hard. Here’s the deal. If we sit with them on the bathroom floor saying “oh buddy, it’s ok, come here, it’s just a little thunder, it won’t hurt you” in your best squeaky, high, lovey voice, we inadvertently tell the dogs there is something to be afraid of! They think their comfort person is afraid too, and the fear is rewarded. Instead, make sure they are safe, make sure they know you are around, and confidently assure them that you’re in the next room if they need you! Gentle, calm, reassurance is the goal.
Once you’ve thought about how you respond to the fear, you can start to work on providing a safe, fear reducing environment. Implementing a combination of these suggestions below can help your dog to relax and be more calm during the storm.
- An interior room if possible
- In a covered crate, but only if he or she is used to being in a crate
- Provide somewhere to “lay low” until the storm passes- a laundry basket, bathtub, corner, or space between couch and wall.
- Classical music or other soothing sounds
- Thunder Shirts are effective for some pets (remember to supervise the first few times! Consumption of the thunder shirt can lead to worse problems!)
- DAP (Dog Appeasing Pheromone) or Adaptil is a calming pheromone
- Composure Pro, or another calming supplement
- A new bone or stuffed kong toy to provide some distraction and positive association
Positive experiences during storms can greatly improve a dog’s response to subsequent storms. Negative experiences, such as being caught in an unexpected storm, being left in a car during a storm, or having an alarm go off during the storm can set them back in their response to a storm.
Some dogs will not respond well to storms despite all of your efforts, and will actually experience worsening anxiety during subsequent storms. For some of these pets, a conversation with your veterinarian about medications to reduce anxiety may be in order. Your vet can discuss medication options with you, and can hopefully recommend a medication that will help your dog to be more comfortable during storms. It’s important to mention that even dogs who are taking medication are unlikely to enjoy or be perfectly relaxed during storms. The goal is to give them some relief from the panic, and allow them reduced anxiety. It’s also important to note that implementing all of the other suggestions in conjunction with starting a medication will usually lead to the best, most effective solution.
You’re not alone! Thunderstorm anxiety is the second most common behavioral concern of dogs, following separation anxiety. Knowing that other pet owners struggle with this stress may not alleviate the frustration and sadness you feel over your dog’s pain, but take comfort in knowing that this anxiety is not your fault. Like people, dogs all have individual personalities, quirks, and struggles. This is part of why we love them so much!
February is Heart Disease Awareness Month for humans, so it seems fitting to talk about heart disease in dogs and cats too! There is enough information on heart disease to fill up many books, so today I’m going to focus strictly on recognizing the early signs of heart disease in your own pets. Recognizing early warning signs is the most important aspect of treatment. Starting treatment early can be lifesaving!
First of all, let me tell you about the best home monitoring tool we have available for BOTH dogs and cats! This is the resting (or sleeping) respiratory rate. Resting Respiratory Rate is the number of breaths that are taken in 1 minute while sleeping or resting comfortably. A normal pet takes fewer than 30 breaths in 1 minute. If your pet is taking more than 30 breaths in 1 minute, it’s probably time for medical attention.
Let’s start with cats, because cats are a lot more challenging. A cat’s main goal in life is to never let on that they have a problem (excluding telling you about an empty food bowl of course!). For this reason, spotting warning signs of heart disease can be tricky! I’m going to talk about a few warning signs, but take note! These can also be signs of other disease processes.
- Open Mouth Breathing: One of the first signs, most pet lovers notice, is open mouth breathing. Cats are termed “obligate nasal breathers” meaning they breathe exclusively through the nose. Breathing with the mouth open or panting should be considered warning signs.
- Abdominal effort: excessive motion of the abdomen while breathing, or sitting with the elbows out and head down and out while breathing are signs of shortness of breath.
- Cough: believe it or not, cats with heart disease rarely cough. Even with lungs full of fluid, cats generally don’t cough the way that dogs do! That being said, if you think your cat is coughing, it’s important to consider this a warning sign as well!
- Hiding, reclusiveness, changes in behavior, changes in appetite, and weight loss: this is why cats are tricky. Sometimes the only signs of heart disease that they show us are signs of general sickness.
- Weight Loss with a good appetite: technically, this is most commonly a sign of hyperthyroidism, a disease common in senior cats. However, one of the greatest concerns associated with hyperthyroidism is heart disease. If you are noticing weight loss in your cat, it’s time for a physical exam and bloodwork.
- No sign or advanced warning at all: unfortunately there are some cats who give absolutely no sign of disease or discomfort until their body is unable to compensate. At this point in time they start showing signs of respiratory distress and require immediate attention.
While we are talking about respiratory patterns in cats, let’s talk about other reasons cats are short of breath or struggle to breathe! One of the more common is feline asthma. This usually results in a “wheeze” or respiratory pattern described as a cough. Generally the head and neck are extended, and they sound like they are “trying to vomit” or “trying to cough up a hairball”. This condition also requires treatment, so if you are in doubt, it’s time to call the vet!
Dogs are similar, but with a few differences. In general dogs are a little easier to recognize the signs. The average dog isn’t quite as stoic as the average cat!
- Cough: unlike cats, the first sign of heart disease that most owners notice is coughing. The cough is non-productive, throaty, and persistent.
- Shortness of breath and exercise intolerance: this is easier to notice in younger dogs. Young dogs who just can’t play like normal young dogs may have an underlying heart condition.
- Fainting or collapse episodes: These are called syncopal episodes, and it usually looks like the dog has fainted.
- Abdominal effort, increased respiratory effort: If the abdomen is moving as much as the chest while the dog tries to catch his breath, or if the pet is standing with elbows out and neck extended, it’s time to seek medical attention.
- Weight Loss, appetite loss, general lethargy: Sometimes pets with heart disease will either have a hard enough time breathing that they don’t want to spend energy eating, or will have behavior changes that result from their discomfort breathing.
- Positive heartworm test: heartworm disease can cause heart failure, so it’s important to keep up with those yearly heartworm tests and routine heartworm prevention. Catching heartworm disease before clinical symptoms are present makes treatment much easier and safer and the risk of long term complications and heart failure are less.
Now let’s talk about common respiratory difficulties in dogs OTHER than heart disease. One of the more common ones that we see is called “reverse sneezing”. This is a relatively normal thing that some dogs will do on occasion. It sounds like “choking” or “coughing”, but is really just an irritation of the nasopharynx. Coughing can or shortness of breath can also be signs of upper respiratory infection or pneumonia. However, if your dog is doing any kind of coughing or shortness of breath, it’s best to have them evaluated by a veterinarian.
Is my expectation that you sit around counting your pet’s respiratory rate and stressing about early warning signs of heart disease? Absolutely not! Is it my hope that you will notice a subtle change in your dog or cat, and the result will be a quicker start to diagnosis and treatment? Absolutely!
Since quarantine started in March, we’ve seen a lot of families decide to add a new pet to their homes. This means it’s time to discuss topics about how to keep our pets healthy, and how to give them long, full lives. Just like humans, it’s much easier to start out eating healthy and exercising and to make a healthy lifestyle a habit, than it is to lose weight and start new habits and activities. Most pets will become overweight in their first 1-2 years of age. During those first two years they stop growing, lose some of their puppy or kitten hyperactivity, and we neuter them and take away the hormonal component of their metabolism. It’s a recipe for weight gain! Unfortunately, there are so many other preventative care topics to cover during those first few puppy and kitten visits, that healthy weight and body condition frequently gets overlooked. In the midst of talking about heartworm prevention, flea and tick prevention, vaccines, and socialization, we forget to talk about diet and exercise! In fact, you might not even think about healthy weight as a preventative care topic. However, discussing the risks of obesity has been shown to be a VERY important topic of health and preventative care!
Way way back in 2002, a study was published showing that in a research population of labrador retrievers, the average lifespan was longer for dogs who were Calorie restricted (i.e. kept thin and trim) compared to their counterparts who were not Calorie restricted. For years this study, called the “Lifespan study” has been a core piece of information regarding the importance of healthy weight. This study does have a few limitations. For starters, this study was done ONLY on labrador retrievers, and ONLY on a research population.
More recently, a study was published in 2018 showing the impact of obesity on a variety of breeds. This study was done using information collected by Banfield Pet Hospital. This national chain of veterinary hospitals has 900 clinics across the country. They collected information on the body condition and lifespan of client owned dogs of 12 different breeds (both large and small dogs). This means the researchers were evaluating data on dogs just like the ones that live in our homes.
This study showed that dogs who are a normal body condition live on average 2.5 years longer than their overweight counterparts. That’s a big finding! In large breed dogs, Labradors, Golden Retrievers, Boxers, and German Shepherds, the split was smaller. Normal body condition dogs lived on average 5 months longer than overweight dogs of those breeds. In smaller dogs such as Chihuahua, Pomeranians, and dachshunds, the normal body condition dogs lived an average of 2.5 years longer. In all breeds, the average life span of a dog of normal body condition was longer than the overweight population.
At this point in time cat owners are wondering what this means for their population of pets! Overweight cats are more prone to diabetes, heart disease, mobility concerns, and urinary concerns. All of these diseases can considerably shorten the lives, and the quality of life, of our feline friends.
Now that I’ve given you a lot of information about why it’s best to keep our pets’ weight down, what do we do about it?
First of all, let’s identify what a healthy body condition looks like! A healthy body condition, for all breeds and species, involves some shape. You should be able to see a curve from the rib cage down to the abdomen, then back out to hips. You should also see a gentle curve up from rib cage to abdomen. You should be able to easily feel the ribs, without being able to see and count them.
If your pet is currently trim, let’s keep them that way! It’s much easier to prevent weight gain, than to take weight off! After young dogs and cats are neutered, and as they reach maturity, their Caloric need is generally not as high. Sometimes a reduction in food is needed when they hit their mature, adult weight. Here’s a few tips for keeping your dog or cat thin!
- Watch treats and snacks! If your pet is highly food motivated, they might be just as enthusiastic about a portion of their dinner used for training and treats throughout the day. The amount that you gave as treats for training comes out of their total Calories.
- Get everyone on board, so everyone in the family knows how much the pets are eating. Tricky pets (Cats are exceptionally good at this!) will trick another family member into thinking they haven’t been fed, or to giving another snack!
- Healthy snacks, like green beans, can be used in place of milk bones and commercial treats.
If your pet is currently overweight, don’t despair! With some good motivation, these pets can lose weight! It can be done! Here’s a few suggestions.
- Cut back the Calories! Reduce the food, cut out table food, and cut back on treats. If treats are an important part of their day, replace the treats with a lower calorie alternative like a green bean, or use part of their dinner as a treat throughout the day.
- Exercise. Even cats can do it! Start small, and with low expectations, and work up. A walk around the block is a good starting point. Cats can be motivated with laser pointers and toys, make sure they get the reward of the catch at least a few times during their play sessions.
- Cats will often have their best weight loss on a canned diet. Dogs may need a prescription Calorie restricted diet if they are really struggling to lose weight. Talk to your veterinarian about these options!
It’s true! Staying trim can help our pets live longer, healthier lives! New Year’s Resolution weight loss isn’t just for people!
 Since March we have heard a lot about “essential workers”. We’ve had the opportunity to think a lot about those around us who perform jobs we simply can’t do without. We’ve watched mail carriers, hospital workers, medical professionals, grocery store workers, and law enforcement be praised and acknowledged for doing things that we simply can’t do without. So it seems fitting to honor and talk about those wonderful people who keep veterinary clinics afloat. The people who are essential to the running of most veterinary clinics, and yet rarely receive the accolades they deserve. Our Certified Veterinary Technicians.
Since March we have heard a lot about “essential workers”. We’ve had the opportunity to think a lot about those around us who perform jobs we simply can’t do without. We’ve watched mail carriers, hospital workers, medical professionals, grocery store workers, and law enforcement be praised and acknowledged for doing things that we simply can’t do without. So it seems fitting to honor and talk about those wonderful people who keep veterinary clinics afloat. The people who are essential to the running of most veterinary clinics, and yet rarely receive the accolades they deserve. Our Certified Veterinary Technicians.
Have you ever wondered about our workflow here at Highland Pet Hospital? While our COVID protocols have changed it a little, the general idea is the same. A veterinary assistant receives the patient, gets a medical history, and enters all the information in the computer. A veterinarian then does a physical exam, comes up with a diagnostic plan, interprets the diagnostics, prepares a treatment plan, and communicates with the patient’s owner. Our technicians, with the help of the veterinary assistant, execute the diagnostics and treatment. This can involve drawing blood, placing an IV catheter, expressing anal sacs, looking at cytologies, staining slides, trimming nails, running bloodwork, taking x-rays, administering medications, keeping IV pumps running, calling owners, filling medications, and administering vaccines. Our technicians are also responsible for making estimates, keeping equipment running, ensuring that workplace safety is followed, and keeping track of medication refills. Sound like a lot? It is! We ask them to keep the workflow running smoothly, and from our client’s perspective, they do this largely behind the scenes!
On a typical day you will see our technicians stationed in a variety of positions, and throughout the week they will hold each of these positions.
- Surgery- our surgery technician is responsible for administering sedation, placing an IV catheter, intubating and prepping the patient for surgery, and for monitoring anesthesia. The surgical technician is also an advocate for the patient, making sure the surgeon is aware when the temperature is getting low, monitoring changes in blood pressure, and making adjustments to maintain a safe anesthetic plane.
- Hospital Admit- our HA technician is a jack of all trades. This person monitors and executes treatments on hospitalized patients. This sometimes means assisting in minor procedures, monitoring critical patients, drawing up and administering medications, and running a variety of lab procedures. They also handle the bulk of incoming communications for owners, and make sure the Doctors have all of their incoming lab work results for the day.
- Exam- our exam technician organizes all of the regularly scheduled routine exams for the day. This means drawing up vaccines, printing rabies certificates, and drawing blood. They also handle all appointments made with a technician. This includes appointments such as anal sac expressions, nail trims, blood draws, and vaccine boosters.
- Prompt Care- the prompt care technician oversees all appointments being seen through prompt care. Frequently this means drawing blood and running lab work, as our prompt care patients are generally sick and requiring diagnostic procedures. Ear cytologies, skin cytologies, bloodwork, and urinalysis are common diagnostic procedures. They may also be called on to assist in minor procedures such as unblocking a cat, laceration repairs, and bandage changes.
We love our technicians. They are the backbone that keeps our hospital running smoothly. They provide the stability and organization that is required to keep up with the busy pace in the hospital. They are animal lovers, animal caretakers, and animal advocates. They are Veterinary Technicians! Shoutout to Casey, Abby, Melissa, Lisa, Jessica and Kolleen! We couldn’t do it without you!
Cats. A unique blend of jungle tiger and purring lap ornament. These personality filled creatures can go from climbing your curtains and exploding around corners to chase the light of a laser pointer to napping in the window for hours. Humans did good work domesticating dogs, but the wild Savannah Lion that lives in your house is really just a smaller version of the original. When it comes right down to it, our domestic cats still retain their hunting drive, their carnivorous nutrition needs, and their stoic nature. The average pomeranian doesn’t retain much from their wolf ancestor, but the average house cat is a different story! As such, feline behavior remains a complicated mess of natural instinct and domesticated preference! One interesting thing we’ve recently come to understand about cats is the impact of “stress” on their systemic body health. Stress isn’t always what we think of as stress, but is more found in lack of outlet for natural behavior (i.e. stalking and hunting instinct) and introduction of unwanted stimulus (such as a new housemate, new baby, new puppy, or a stray cat hanging around outside). “Stressed” cats are more likely to be frequent vomiters, exhibit play aggression, and have inappropriate litter box habits. In fact, stress is the primary factor we attribute to Feline Lower Urinary Tract Disease (FLUTD, sometimes called sterile cystitis, or stress induced cystitis). FLUTD causes blood in the urine, straining to urinate, urinary indiscretion, and in male cats can cause urinary obstruction. Another thing that many vets and cat owners find to be extremely frustrating is the stoic nature of cats. Unlike dogs, who frequently cry and limp for days just because they split a toe nail, our feline friends frequently don’t show any sign of illness or pain until they simply can’t compensate any more. At this point, cat lovers sigh, shake their heads, and say “oh cat, you really could have told me sooner.”
What does all this have to do with declawing? Well, feline medicine is constantly evolving as we try to figure out the enigma of the cat. One of the more recent things to come under intense scrutiny is the practice of declawing cats. At Highland Pet Hospital, we strive to do the best we can for our feline patients, and this means following all the recommendations and updates made by the American Association of Feline Practitioners, and the American Veterinary Medical Association. AAFP and AVMA have been scrutinizing the practice of declawing cats for some time now, and Highland’s doctors have come together to also think long and hard about this procedure.
As of March 2020, Highland’s doctors have decided to no longer offer the declawing procedure at our clinic. There are many reasons for this, and we’ve spent a great deal of time thinking about them!
One important reason is that declawing is considered an elective procedure that does cause pain and permanent alteration without a medical benefit to the patient. Declawing (Onychectomy) is the surgical amputation of the last bone of each toe. It does cause pain, it is stressful (as all surgeries are) and there is a risk of complication. Complications include chronic pain, damage to the paw pads, and infection. Since cats are so stoic, it is very possible that we underestimate the discomfort they feel from this procedure. The few cats who show chronic pain may just be those who feel it the most severely. We have to assume that there is a subset of cats who are more severely affected by the after effects of mental stress and pain than they let on! The procedure also involves anesthesia, so all of the possible complications of anesthesia exist as well.
Another reason we’ve decided to discontinue the practice of performing declaws is due to the disruption of natural behaviors. Scratching is a natural behavior, and cats who have been declawed do show increased tendency toward biting (as opposed to scratching) when afraid or angry. There is also the possibility of stress related behaviors such as urinary indiscretions, hiding, and aggression.
Finally, Highland’s staff strives to invest more time in the things we are passionate about and to move away from things that don’t further our mission statement of Healing, Health, and Hope for Pets, their People, and Our Community. As a team, we have decided the declawing procedure was not something that drove us, and did not further the goals we have determined to be important to us.
With all that being said, we also recognize how very frustrating naughty cats and their sharp claws can be. Those claws can be quite damaging to property, other pets, and to our own skin! One thing that we are all passionate about is education. So, in light of our decision not to perform the declaw procedure, we are working on offering more education in the natural scratching behavior of cats, and how to work with it. Each new kitten family will be able to communicate with one of our vets or with one of our staff members about the natural behavior of scratching, scratching posts, and discouraging scratching in inappropriate places. We have also set a goal of demonstrating nail trimming to all of our new kitten families (though this has proved to be an unexpected challenge in light of COVID 19, we hope to be more organized about meeting this goal as we are more free to allow pet owners to accompany their pet into our exam rooms). We are also offering a free application of Soft Paws to all of our kittens. Soft Paws are claw covers, which can be applied at home. One of our team members will demonstrate the application process for you, it’s surprisingly easy! These are a safe alternative to protect your skin and your property, and are widely accepted by most cats!
We recognize that most pet owners will see this as an acceptable move toward better medicine for our feline friends, and that some pet owners will find this to be a difficult change to understand. As such, we welcome and encourage conversations between cat owners and their veterinarian! Ultimately we all want the best for these tiny panthers with which we share our homes. We may never understand them, but that’s part of their charm!
 Over the last month the world has entered a collective hibernation. People are going without haircuts, cutting grocery store visits down to once a week, ordering food to go, and entertainment of all types has been indefinitely postponed. While we humans are adjusting to having our social lives wrecked, our dogs are celebrating our increased presence in their lives. Cats give the quarantine mixed reviews. While it’s popular among some cats, half of the feline population misses uninterrupted day naps.
Over the last month the world has entered a collective hibernation. People are going without haircuts, cutting grocery store visits down to once a week, ordering food to go, and entertainment of all types has been indefinitely postponed. While we humans are adjusting to having our social lives wrecked, our dogs are celebrating our increased presence in their lives. Cats give the quarantine mixed reviews. While it’s popular among some cats, half of the feline population misses uninterrupted day naps.
Interestingly, Highland Pet Hospital has seen a huge increase of new puppy and new kitten visits, as well as recent shelter adoptions of older dogs and cats. While we would normally see an increase in new pets at the start of spring and summer, the influx of new pets we are seeing right now is seeming to be higher than usual at this point in the year. It’s a good time to add a pet, especially a young one. After all, increased time at home means more time for training, more time for bonding, and a good opportunity for companionship when human contact is very limited.
But here’s the thing:
There is a life after COVID-19. The quarantine will end, and all of our Covidogs and Coronocats will have to experience a major life change when the world starts back up. While I’m mostly focusing on new additions to the family, the reality is ALL dogs and cats are going to experience an adjustment back to normal life once we all go back to our usual bustling lives! Here are a few thoughts I’ve been having on preparing our pets for life after COVID-19.
Keep up with vaccines—
Veterinarians across the country are sticking to “essential” veterinary care, which makes appointments harder to schedule, and makes it very likely that there will be delays in vaccine coverage. We are trying to prioritize rabies for all pets, and the distemper combination for puppies who have not yet had the vaccine. Parvo virus is VERY real, and a VERY big threat. Avoid exposing an unvaccinated puppy to other dogs until those vaccines are updated! If you have a new puppy or kitten, call and make an appointment! We will do our absolute best to see your pet, while trying to keep all the people safe as well. Similarly, vaccines like bordetella (kennel cough) that are recommended for grooming, day care, and boarding may lapse as we are not considering them essential right now. Remember to get these vaccines updated before your dogs make their way to daycare!
Clarify any questions or concerns you have for your veterinarian-–
what we are calling “curbside medicine” results in significantly decreased face to face communication with your veterinarian. As a new puppy or kitten owner, you may have many questions. An unfortunately byproduct of being asked to wait outside during your pet’s examination is that you may have questions that you forget to ask, or your vet forgets to comment on! We feel just as sad at the decreased contact as you do, and we are more than happy to answer general questions about care for your new puppy or kitten! At Highland we actually have some people who are working from home, with the sole job of responding by email to questions from our clients!
Socialization is a challenge right now-–
Normally, my leading advice to new puppy and kitten owners is to have them meet as many people as you can during those first months. Handling by people during the early months is SO important. Unfortunately, I cannot currently offer that piece of advice. But never fear! I have some alternatives for you!
→→Spend a lot of time handling your pet. Touch paws, ears, and mouths. Handle their toe nails, open their mouths, lift their lips, look in their ears. Work on laying them on their sides, petting them, and rolling them over on their backs. The more, the better! ←←
→→Work on basic obedience training. Having a good handle on basic commands is so good for young animal’s brains, helps them to burn energy, and will allow you to have a good trust with them once they are able to meet new people! ←←
→→For cats, look up some information on the needs of indoor cats for environmental enrichment. I like indoorpet.osu.edu/cats as a resource for information on cat behavior. You can start to implement things like soft paws and scratching posts early on to get ahead of negative behaviors. For extra entertainment, check out Jackson Galaxy’s you tube videos! Jackson Galaxy has some really fun information on cat behavior! He hits some topics a little harder than I generally would, so if you run across something you have questions about, your veterinarian may be able to clarify! ←←
→→If your quarantine crew includes multiple family members, make sure everyone has an equal role in training and handling. Since the number of people your pets can meet outside the home is limited, those who live in the home are even more valuable for socialization! Use discretion with young children, and always supervise the interactions of kids with animals. ←←
Make sure your puppies are crate trained, and your kittens know how to spend time away from you.
⇛I’ve saved the most important for last! ⇚
In a few weeks those who are working from home will go back to work, or will want to have a nice dinner out. Separation anxiety is the behavioral problem we are asked to address more than any other. It is so important that puppies be crate trained, so that they have a safe place to stay when unsupervised. All pets should spend some time being content away from you each day. This allows them to be adjusted to being alone once the house finally empties out. I can’t emphasize the importance of crate training and preparing your puppy to be home alone enough! You will appreciate a puppy who is content and safe in a crate while you are out of the home. You will also appreciate a puppy who knows how to be content in a crate even when you are home! Eventually we will be able to have dinner parties again, and it’s very handy to have a place for the pets to go while you have guests!
We all need a little extra good news, a little more love, and a lot more companionship during this isolating time. I think all of our pets have the potential to benefit greatly from our increased attention! Let’s set them up for success during the time after the quarantine!
Did you ever know you would be spending so much time thinking about infectious disease? As COVID-19 grips the world, many people are learning more about viruses and infectious disease than they ever wanted to know. While COVID-19 does not infect our pets, there are a number of infectious diseases that DO cause serious illness in our companion animals. Fortunately, many of the most devastating diseases have vaccines that help to keep our pets safe. It can be easy to get overwhelmed and lost in the vast number of recommendations for vaccines. Since most of us who work at vet clinics abbreviate the vaccines names, it can be hard to know the ABCs and LMNOPs of DAPP, DAP, Lepto, H3N2, and FVRCP.
Let me outline Highland Pet Hospital’s vaccine protocol for you.
Note that vaccine protocols will vary between clinics. This doesn’t mean one is right and one is wrong! Different geographic regions may have different recommendations, different pricing structures and doctor preference may alter how vaccines are given. This is ok, and means that the vets involved have given some thought to how best to keep your pet safe.
Dog vaccines at Highland are grouped into two categories.
First, Core Vaccines. Core Vaccines are Rabies and a combination vaccine called DAPP. A 1 year rabies is given to puppies, and repeated at the one year visit. At the two year visit, we start giving a 3 year rabies vaccine. The so called “DAPP” vaccine is for Distemper (a viral infection that affects respiratory tract and neurologic system), Adenovirus (a viral infection that affects the liver), Parainfluenza (a viral upper respiratory infection), and Parvo (a viral infection of the intestinal tract). After the first two years, the DAPP vaccine is separated out and rotates with the rabies vaccine so that dogs get Rabies, Parvo, and DAP in a three year rotation. In this way, we try to prevent over vaccination and allow for the greatest immune response to the vaccines. At Highland, all core vaccines are paid for with your annual wellness exam.
Second, a class of vaccines we call “social vaccines”. Social vaccines are evaluated based on the patient’s risk. Not all dogs will need to have these vaccines. The majority are needed by dogs who are in contact with other dogs, usually through boarding, grooming, or day care. These are bordetella (known more commonly as kennel cough) and CIV (or canine influenza virus). Bordetella and CIV cause upper respiratory signs, particularly coughing. The other vaccine we administer according to risk is called Leptospirosis (or lepto). This is a bacterial infection that is transmitted in urine. As such, dogs who are at risk are those in contact with water through hiking, runoff, streams, retention ponds, and garden ponds and those dogs who are in contact with wildlife. We do occasionally vaccinate for Lyme disease, but as Lyme disease is just one of the diseases carried by ticks, I tend to prefer a good flea and tick preventative protocol over vaccination for Lyme disease. Social vaccines are all included in a package that is purchased once yearly.
Cats are a little easier.
Core vaccines for cats are Rabies and a combination vaccine called FVRCP. We do try to be very careful with vaccine injections in cats, as cats are prone to a type of tumor that can develop at the injection site. Because of this, we select vaccines that do not have “adjuvent”. Adjuvent is included in some vaccines to enhance the body’s response to the vaccine, but cats’ bodies respond badly to adjuvant. Our rabies vaccine is non-adjuvented, and is given yearly. FVRCP stands for Feline Viral Rhinotracheitis, Calicivirus, and Panleukopenia. Rhinotracheitis is the feline herpes virus. Rhinotracheitis causes severe upper respiratory signs and ulceration of the cornea. Calicivirus causes upper respiratory signs as well, but the ulcerations are generally in the mouth. Panleukopenia is commonly referred to as feline distemper, and causes a variety of clinical signs. We have chosen an intranasal FVRCP vaccine, which is given into the nose to reduce the number of vaccine injections that need to be given to a cat. FVRCP is given every 3 weeks to kittens, repeated at 1 year, and then given every 3 years. The only elective vaccine for cats is a feline leukemia vaccine, which should be given to all cats who spend time outdoors. Feline leukemia is transmitted by exposure to cats who are carrying the disease. All feline vaccines are included in the cost of the annual exam.
Vaccines are extremely important to prevention of infectious disease. Rabies, though rare, is still seen in wildlife in the United States. Parvovirus is a deadly disease that is almost exclusively seen in dogs who have not been vaccinated. So, it is important to schedule an annual wellness visit with your veterinarian. At that visit you can discuss your pet’s lifestyle and determine which vaccines are most needed, and when they should be given.
Having a hard time getting your pet in for vaccines due to social distancing and quarantine? At Highland we will prioritize appointments and vaccine needs to the best of our ability. Sick pets come first. Pets needing rabies vaccines and puppies and kittens who have not yet been vaccinated will be our top priorities. Pets who are not due for rabies, and have previously had their core vaccines will not be considered priority during the quarantine period. This can seem scary, but never fear. Social distancing for people is also protecting our pets, as dogs and cats will not be boarding, grooming, or going to daycare during this time and thus not exposing themselves to infection. As restrictions on what is considered “essential” change, we will make every effort to have your pets seen promptly. During the quarantine period, our staff will always be available by phone and email to answer any questions you have! As a veterinarian, I feel constantly prepared to fight infectious disease! Join me in the war by vaccinating your pets, (and by washing your hands!)
 When would you say is the start of flea and tick season? How about mosquitoes? One of the byproducts of temperamental central Illinois weather is that the life cycles of our creepy crawly friends are unpredictable! Fleas, ticks, and mosquitoes (all of which pose significant threats to our canine and feline friends) are pretty resilient, and they like to show up well before we are expecting them.
When would you say is the start of flea and tick season? How about mosquitoes? One of the byproducts of temperamental central Illinois weather is that the life cycles of our creepy crawly friends are unpredictable! Fleas, ticks, and mosquitoes (all of which pose significant threats to our canine and feline friends) are pretty resilient, and they like to show up well before we are expecting them.
Why are preventatives important?
Fleas can carry blood borne diseases for cats. Ingestion of fleas is one of the primary ways cats get tapeworms. Fleas love living in our homes, and will continue to reproduce in homes during the winter (we love our heated homes, and so do fleas!). Ticks carry a variety of diseases including lyme disease, ehrlichia, and anaplasma. There is a vaccine for lyme disease, but the others do not have vaccines available and are just as bad (if not worse). Mosquitoes carry heartworm disease. Preventatives for heartworm disease actually work to keep the larval heartworms (called microfilaria) from reaching maturity. This actually means the preventative is working to prevent last month’s exposure from reaching maturity and causing disease. Furthermore, it takes 6 months for a test to be positive! A pet who is infected in March wouldn’t have a positive test until September!
What can you do about these parasites?
Flea and tick prevention and heartworm prevention should be administered year round. There are a lot of options, and not all preventative plans will fit all pets! On the bright side, there are lots of options! The tough thing is that a lot of options can result in a lot of confusion.
What is available and what do you need to know?
Cats
In our area, I prefer the Feline Revolution. I like it because it is administered topically, and has the widest spectrum of coverage. You do need to be cautious of over the counter products, as these often have a harsher active ingredient. Some dog products are HIGHLY toxic (even deadly) to cats.
| Product | Administration | Benefits |
| Revolution | Topical, monthly | Fleas, ticks, mites, intestinal parasites, and heartworms |
| Bravecto | Topical, every 90 days | Fleas and ticks |
| Frontline | Topical, monthly | Fleas and ticks |
Dogs:
I could do pages on pages of notes on the differences in preventatives for dogs! There are so many options, with so many different benefits. I like Heartgard for heartworm and intestinal parasites prevention. Heartgard comes with a very good reimbursement policy in the event of heartworm infection while taking the preventative. Although this isn’t common, if it does happen, the company will cover treatment (and treatment is quite expensive, especially for a big dog!). This only applies if the preventative has been purchased from a veterinarian, given year round, and appropriate yearly testing has been performed. Another important option that you can be familiar with is a yearly (that’s right, YEARLY) injectable heartworm preventative called Proheart. Proheart’s biggest plus is that it is given once yearly, so you don’t have to remember to give preventatives for heartworm disease. In comparison to Heartgard, it doesn’t have quite the same spectrum of prevention against intestinal parasites. The Proheart we carry is only for dogs over 1 year in age, and we don’t recommend it for pets who are sick or at increased risk for autoimmune disease. For fleas and ticks I like Nexgard, which is an oral preventative given once monthly. I like these oral preventatives because they just seem to be more effective, especially for treating an active flea infection. The chart below is just a few of our more commonly prescribed options.
| Product | Administration | Benefits |
| Heartgard | Oral, monthly | Heartworm, roundworm, and hookworm |
| Proheart 12 | Injectable, yearly | Heartworm, hookworm |
| Nexgard | Oral, monthly | Fleas and ticks |
| Bravecto | Oral, every 90 days | Fleas and ticks |
| Revolution | Topical, monthly | Heartworm, SOME ticks, fleas, ear mites, sarcoptic mange
** great for very small dogs and dogs with food allergies |
| Advantage Multi | Topical, monthly | Heartworm, fleas, roundworm, hookworm, whipworm, and sarcoptic mange |
| Frontline | Topical, monthly | Fleas and ticks |
| Advantix | Topical, monthly | Fleas and ticks, biting flies, chewing lice |
If you’ve ever heard the phrase “an apple a day keeps the doctor away”, you’ll understand why preventatives are so important. A preventative a month keeps the crawlies away!
What Pet Owners Should Know
Part 1
As of January 1, 2020, recreational marijuana use will become legal in Illinois. It’s been a topic of hot discussion for a long time, but what you might not know is that veterinarians expect to be impacted by this change as well! I expect we will see some problems with increased access to recreational marijuana, but I actually think there will be a net benefit. Before we discuss what I expect to be good and to be bad, let me give you the rundown on marijuana.
Cannabis- This is the genus of plant from which marijuana and hemp are obtained 
Marijuana- dried flower from a type of Cannabis plant, this contains many cannabinoids including THC and CBD.
Hemp- a variety of cannabis plant, but the THC content is lower than in marijuana plants. Instead CBD is the Cannabinoid present in the highest quantity.
Cannabinoids– components of the cannabis plant (and some other plants!) that bind to certain receptors in the brain.
The two most common, and most readily studied, cannabinoids are THC and CBD
THC– (delta-9 tetrahydrocannabionol) This is the psychoactive component of marijuana. It does have a lot of anti-inflammatory components, appetite stimulating components etc. This is what gives users the “High”
CBD– (cannabidiol) This has many benefits in the body, without the psychoactive component. It helps to counterbalance hunger, lethargy, anxiety and high heart rate caused by THC.
Animals are quite sensitive to THC, and are much more susceptible to the negative effects of this component of Marijuana.
A dog exhibiting THC toxicity will show the following signs:
— Lethargy
— Ataxia
— Vomiting
— Tremors
— Hypothermia
— changes in heart rhythm (sometimes slow, sometimes fast)
— low blood pressure
— Disorientation
— Drooling
— Vocalization
— Urinary incontinence
A Cat exhibiting Marijuana toxicity will show the following signs:
— Dilated pupils
— Drooling
— wandering aimlessly, spontaneous jumping, sometimes switching between lethargy and spontaneous movement.
— sedation
— head bobbing
— ataxia, swaying side to side
— vocalizing – meowing, hissing
— aggression
Marijuana toxicity is treated symptomatically, meaning that we manage low body temperatures, treat seizures or tremors, treat changes in heart rhythm, and maintain blood pressure.
One concern associated with legalization of recreational marijuana is that pets will be more likely to be exposed. While increased accessibility may result in a slight increase in marijuana ingestion cases, I still think the end result will be beneficial to pets and their vets. Up to this point, determining that a pet has indeed ingested marijuana is often a struggle. It’s hard to admit that an ingestion of illegal substance could have occured, even when it’s in the best interest of the pet. In some cases the owner of the pet may be unaware that there was potential exposure because other members of the house, friends etc. may be less forthcoming about illegal substances.
On the other hand, states that have already legalized marijuana report owners willingly calling to report their pet had consumed THC containing product. Owners are willing to tell their vet about the exposure without fear of repercussion or judgement. This allows correct treatment to be initiated promptly. It also allows the vet to use additional resources, such as animal poison control, for help in executing correct treatment. Overall this leads to less frustration, more accurate treatment, and improved outcome.
I am hopeful that we will not see an increase in marijuana toxicity cases, but will find that accidental ingestions are easier to identify and treat as people feel more free to discuss the potential exposure of their pet to THC containing products.
You might have some ideas about what your pet is thankful for, but what do you think your vet is thankful for? You might be surprised by how often pets and vets are thankful for the same things!
The Dog: I’m thankful for a big backyard to run and play in. I’m thankful for squirrels to chase and bark at.
The Vet: I’m thankful when pets have opportunities to exercise. Plenty of times to run and play makes for dogs that are physically and mentally healthy.
The Cat: I’m thankful for long naps in my warm bed. I’m thankful that no one disturbs me while I’m taking my nap.
The Vet: I’m thankful for cats with enough resources to have their needs met. That means appropriate litter boxes, plenty of water sources, things to play with, and comfortable resting places. Having adequate resources reduces a cat’s stress level, and can prevent stress related diseases such as behavioral inappropriate urination and lower urinary tract inflammation.
The Dog: I’m thankful for food! Milkbones, foods, treats, snacks, and dinner!
The Vet: I’m thankful for owners who choose healthy diets and snacks for their pets. I’m also thankful for owners who keep their dogs and cats from eating too many of their favorites snacks. A treat should be just that… a treat.
The Cat: I’m thankful for my lovely coat, and I’m thankful for my daily hair maintenance routine. Who needs shampoo when you have a nice rough tongue!
The Vet: I’m thankful for cats who are able to groom themselves. I see it as a warning sign when a cat stops grooming themselves. It can suggest joint pain, illness, or even obesity.
The Dog: I’m thankful for my daily walks, my visits to the dog park, and my social routine at Doggie Day Care. I’m thankful for other dogs to play with, and for the ability to stretch my legs.
The Vet: I’m thankful for dogs who get to interact with other dogs and with other people. There is a lot of benefit both mentally and physically. This is why I recommend vaccines! One coughing pup can be risky to everyone!
The Dog: I’m thankful for my human. I love when my human scratches my ears, rubs my belly, fills my bowl, and takes me for walks. I’m thankful for when my human comes home and I get to wag and bark and wiggle for joy!
The Cat: I’m thankful for my human. I love napping together on the couch, I love when my human fills my bowl, and I love a clean litter box! I’m thankful when my human gives me a new box to play in, or shows me a new toy.
The Vet: I’m thankful for their humans. I’m thankful for animals who have a forever family to love them and provide for their needs. I’m thankful for animals who learn trust and loyalty to their people. I’m thankful for people who are willing to care for animals in sickness. I’m thankful for people who desire to keep their pets healthy. I’m thankful that animals can feel loved by humans, and in return humans can feel loved by animals. The bond between people and animals is amazing, and I’m thankful for it.
What are all these lab tests, and why are they necessary?
Chemistry may remind you of your least favorite subject in school, or it might sound like a science experiment. To your veterinarian, a “Chemistry Panel” can provide a LOT of valuable information! Here are a few common lab tests that might be recommended by your veterinarian, and why they are important to the health of your pet.
- Chemistry Panel: this panel tells us about glucose, kidney values, liver values, protein levels, and electrolytes.
— From this, we could potentially catch diseases from diabetes to kidney disease before your pet even shows signs of illness! 
— Some bloodwork is useful for finding new diseases, and some bloodwork is needed for monitoring medications and chronic diseases.
— A fresh blood sample is required for this test
- Complete Blood Count (CBC): this panel tells us about white blood cell count, red blood cell count, and platelet count.
 — from this panel we can catch infection, anemia, and other conditions. It is also very helpful to know trends in these values from year to year!
— from this panel we can catch infection, anemia, and other conditions. It is also very helpful to know trends in these values from year to year!
— from this panel we can catch infection, anemia, and other conditions. It is also very helpful to know trends in these values from year to year!
— A fresh blood sample is required for this test
- Heartworm Test: this is a test for canine heartworm disease (a blood parasite)
 — although heartworm disease is less common than some other parasitic infections, we are seeing an increasing rate of infections in our area.
— although heartworm disease is less common than some other parasitic infections, we are seeing an increasing rate of infections in our area. 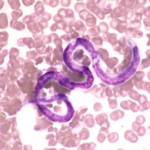
— Luckily, heartworms are highly preventable. It takes 6 months from the time of the mosquito bite for the test to be positive, which is one reason why yearly heartworm testing is the best way to catch an infection.
— a heartworm test is recommended prior to starting heartworm preventative and annually to assess for prevention failure.
— A fresh blood sample is required for this test
 — most intestinal parasites can be transmitted to people and to other pets, so it’s a great idea to catch infection early and treat before allowing too much opportunity for spread!
— most intestinal parasites can be transmitted to people and to other pets, so it’s a great idea to catch infection early and treat before allowing too much opportunity for spread!
— pets who are losing weight, having diarrhea, or vomiting may need to have a stool sample checked.
— A fresh stool sample is recommended for this test
 — from this test we can monitor for signs of endocrine diseases, such as diabetes, kidney disease, and urinary tract infection. We can also monitor urine concentration.
— from this test we can monitor for signs of endocrine diseases, such as diabetes, kidney disease, and urinary tract infection. We can also monitor urine concentration.
— A fresh urine sample is required for this test
— There are several ways to go about collecting a sample. Your veterinarian can discuss these options with you!
- Thyroid testing: this test examines for inappropriate amount of thyroid hormone
 — dogs are more prone to hypothyroidism, while cats are more prone to hyperthyroidism.
— dogs are more prone to hypothyroidism, while cats are more prone to hyperthyroidism.
— a hyperthyroid cat will lose weight rapidly, and can have secondary complications such as heart disease.
— a hypothyroid dog will gain weight, and can have secondary complications such as panting, skin disease, and muscle weakness.
— A fresh blood sample is required for this test
The tests listed above are our most frequently requested tests. Other tests may be indicated, but are not routinely run on each patient. Lab work can sound intimidating, but is an important part of routine health care for our cats and dogs!
A few do’s and don’ts on enjoying the weather with you dogs.
Summer Heat Guidelines:
- Some breeds don’t tolerate the heat well
- Thick coated breeds- collies, huskies, malamutes, newfoundlands
- Large Breeds- great danes, rottweilers, boxers
- Bracycephalic breeds- pugs, french bulldogs, boston terriers
- No cars. Period. It’s unimaginably hot in a closed car. Don’t be tempted, it’s not worth the risk
- Some dogs don’t know when to quit
- Dogs who love to please won’t quit, even when they get tired.
- Limit exercise for those who would chase a ball until they drop
- The pavement is HOT!
- If you wouldn’t walk on the pavement barefooted, your dog probably doesn’t want to either. Pawpads can be burned by hot pavement.
- Give them a place away from the sun.
- You may like soaking in the rays, but dogs need shade and plenty of water during the heat of summer.
- If your pet is used to air conditioning, they aren’t going to be as tolerant of the heat.
Fun things to do with your pets this summer
- Go for a swim
- Start small. Not all of us are natural golden retrievers! There is nothing wrong with a few inches of water in the bottom of the kiddie pool as a starting spot. Small plastic pools are pretty affordable, and are a great way to introduce your dog to water. Don’t force reluctant pets. They’ll do what they are comfortable with.

- Start small. Not all of us are natural golden retrievers! There is nothing wrong with a few inches of water in the bottom of the kiddie pool as a starting spot. Small plastic pools are pretty affordable, and are a great way to introduce your dog to water. Don’t force reluctant pets. They’ll do what they are comfortable with.
- Learn a new trick
- When the family is home from school, it’s a great time to learn some new tricks. You don’t have to be outside to do some obedience training. If you are beating the heat outside by hanging out in the air conditioning, take the opportunity to brush up on Fido’s obedience training.
- Bobbing for treats
- Remember that kiddie pool? Fill with a few inches of water, and drop treats one at a time into the water. Active dogs will enjoy fishing the treats out. Remember not to over do it on the treats OR the water! Yes, there is such a thing as drinking too much. No upset bellies this summer, please!
- Challenge your dog’s nose
- Start small by having your dog stay, place the treat a few feet in front of them, and make them wait until you say “find it.” Gradually move the treat further, then start hiding. Another alternative is to play “find the treat” using three shoeboxes and a strategically placed snack. These are good games to keep the mind occupied.
- Don’t fear the walk!
- As long as you exercise caution, walks can be a safe summer activity. Do outdoor activities in the morning and evening, and don’t take a fast walk. Take a nice, short stroll. Be sure to stay off hot pavement, stay in the shade, and take some water.
What you should know about Heat Exhaustion and Heat Stroke
- Symptoms
- Bright red mucus membranes, collapse, excessive panting, vomiting, and seizures can all be signs of heat stroke. A rectal temperature over 104 degrees after exertion is suspicious for heat exhaustion
- What to do
- Start cooling. Wet paw pads with cool water, hose dog with cool water, and start a fan on the dog. This can be life saving. Cooling should be stopped when the pet reaches 104 degrees to avoid dropping the body temperature too low.
- HEAD TO THE VET RIGHT AWAY
- Complications of heat stroke
- Renal failure, interruptions in the ability of the blood to clot, and hypoglycemia can occur. Unfortunately pets that suffer from heat stroke are at a very high risk of developing complications that result in death.
The Cost of a Free Puppy
Some honest thoughts on the cost of veterinary medicine, and how to be prepared for the costs of health care for your best friends!
In my previous posts, I have given some information relevant to pet owners. My intention has been to give information that pet owners would find useful, and interesting. I hope that this post will be as informative as the previous posts, possibly even more so. I’m going to tackle the sensitive subject of the cost of pet ownership. I recently read an article from CNBC. This article makes reference to a report from the People’s Dispensary for Sick Animals. This report says that an astounding 98% of people underestimate the lifetime cost of pet ownership. As a collective whole, veterinary clinic team members recognize the financial constraints of pet owners. In order to combat this problem, we need to be prepared.
What are the costs?
New Pet care– spay/neuter, puppy vaccines, microchip
Routine care– annual physical exams, annual vaccinations, heartworm preventative, flea and tick preventative, heartworm testing, and diagnostic monitoring profiles
Sick pet care– vomiting, diarrhea, coughing, mild musculoskeletal injuries
Emergency pet care– foreign body surgery, severe GI disease, hit by a car, toxin ingestion, laceration repair, bloat (GDV), anemia (low blood volume),
Orthopedic concerns– ACL tear (Knee injury), fracture, neck/back injury, hip dysplasia
Chronic health concerns– diabetes, hyperthyroidism, Cushing’s disease, Addison’s disease, renal failure, heart failure, arthritis, ears
Allergies– deserving of a category to themselves! This may involve medications, diet changes, and frequent medications for skin infections.
— to name just a FEW!
How can we be prepared?
Certainly not all pets will develop all of these diseases, but when an emergency or a chronic illness arises, it’s good to be prepared.
- Understand how expensive pet ownership can be. In this way you avoid the shock of expensive veterinary bills. Small breed dogs will be with you for 13-16 years, large breed dogs from 10-12 years, and cats can be a member of the family for as long as 18-20 years. As they age, cost of care generally increases.
- Do some research! Before you buy or adopt, talk to some people who own the type of dog or cat you are interested in. Some breeds have an increased prevalence of diseases such as allergies, back problems, diabetes, ear problems etc. It is good to be mentally prepared for the unique challenges of the breed you select.
- If using a breeder, ask some questions. Ask about the health history of the parents of the pups. Ask about genetic disease testing such as degenerative myelopathy for corgis, collie eye anomaly for herding breeds, and OFA certification for hip dysplasia (and more!)
- Start setting a few dollars a month away. It’s the same concept as an emergency fund for your family, but this is for your fur kids!
- Pet Insurance. It’s a confusing topic, but getting your new pet started on insurance can save you from a heartbreaking situation on down the road.
- Most importantly, don’t underestimate the money saving potential of good preventative care! A few good examples- heartworm preventative is expensive, but it’s cheaper than treating a large dog for heartworm disease. Spaying your dog can prevent uterine infections that lead to emergency surgery. Vaccinating for parvovirus protects your dog from a disease that can lead to several days of intensive care hospitalization!
The report from People’s Dispensary for Sick Animals also states that 93% of people said the decision to own a pet made them happier! We know you love your pet. We don’t really like talking about money, and we certainly don’t like asking for it. As members of a veterinary care staff, we consider ourselves a team, and we want to include you in the team. You, as the owner, caregiver, and all around pet parent are the most important member of the team, and we don’t want to leave you behind. We care about each member of the family, both two legged and four legged!
(Reference- www.cnbc.com , Zack Guzman, http://www.cnbc.com/2017/04/27/how-much-does-it-cost-to-own-a-dog-7-times-more-than-you-expect.html
What dog owners should know about this mysterious, and serious, disease.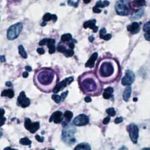
Blastomycosis. Chances are, you’ve never heard of it.
If you have heard of it, you know this little yeast organism is a foe that should not be underestimated!
What is it?
Blastomycosis, commonly called Blasto, is a fungal organism that is found in the soil in the east-central USA. Like most fungi, it likes cool, moist, dark conditions.
Who can get it? 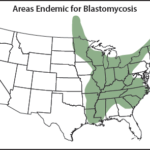
People and Pets are susceptible to Blasto. Dogs are most commonly affected, as they are the most likely to have noses down in the dirt. However, people can pick up Blasto as well! Fungal organisms are inhaled, and convert to the yeast form at body temperatures. Blasto is NOT directly contagious between pets, or between pets and people.
What does it do?
This organism has some favorite locations in the body.
— Pulmonary: when the lungs are affected, the organism causes multiple lesions throughout the lungs. Cough, fever, difficulty breathing, and lethargy are the most common complaints. A severely affected patient will likely need hospitalization, treatment is long, and the prognosis is guarded. 
— Lymph nodes: Like pulmonary blasto, this is a severe infection requiring an extended treatment period. Usually blasto has affected another area of the body, not just the lymph nodes.
— Eyes: one or both eyes can be affected. Initially, we notice inflammation and a low intraocular pressure, but the inflammation quickly progresses to glaucoma (or high pressure). In many cases, the affected eye loses vision. In some cases, the eye must be removed to bring comfort to the patient.
— Bone: this creative organism is well adapted to cause painful lesions in the bone. It can look like bone cancer, so it is important to distinguish between the two.
— Skin: any non-healing wounds, draining tracts, or unexplained wounds should be suspect for blastomycosis.
What should I look for?
Blasto has a very wide variety of clinical signs. Coughing, fever, lethargy, inappetence, vomiting, difficulty breathing, and collapse can all be signs. Enlargement of lymph nodes, squinting/pain in the eyes, oozing skin wounds and lameness may also be noted in some patients. When in doubt, have your pet examined by a veterinarian.
How is it diagnosed?
Most commonly Blasto is most commonly diagnosed by looking for a specific byproduct of the organism (antigen) in the urine. This test is run by an outside lab. Blasto can also be seen in needle aspirates of wounds and lesions on the skin in some cases. X-rays should be used as a tool to evaluate lungs for lesions typical of blasto.
How is it treated?
Treatment takes a LONG time. The core of treatment is through use of strong anti-fungal and anti-inflammatory medications. Each individual patient will be treated differently based on the body system that is affected by the organism.
Learning About Lab Work!
We can learn a lot from a thorough history. That’s why when you bring your pet to the vet you will have to answer a lot of questions (sometimes more than once!). We can also learn a lot from a physical exam. Sometimes the physical exam is enough to give the answer! However, we can gain a LOT of information from running some lab work. Your vet may recommend bloodwork be performed when your pet is sick, as a screening prior to anesthesia, or just as part of a routine annual exam. Today we are going to focus on what we can learn from bloodwork performed as part of a routine annual exam!
Let me start by going through the recommendations that Highland Pet Hospital makes for each species and age group of pets.
Puppies (those under 1 year of age) have a recommendation of a fecal exam.
Adult dogs (1-7 years of age) have a recommendation of a heartworm test, yearly fecal exam, CBC, and abbreviated chemistry panel.
Senior dogs (8 years and up) are recommended to have a heartworm test, CBC, Chemistry (our default panel is a shortened panel, but in some cases a more thorough chemistry panel is indicated), and a urinalysis. A yearly fecal exam is also recommended.
Kittens (under 1 year of age) are recommended to have a FeLV/FIV test and a fecal test.
Young Adult Cats (1-2 years of age) are recommended to have a urinalysis and a yearly fecal test.
Adult Cats (4-8 years of age) are recommended to have a urinalysis, CBC, and abbreviated chemistry panel. A yearly fecal test is also recommended.
Senior Cats (9 years and up) are recommended to have a urinalysis, CBC, chemistry panel, and a Total T4. As with the other age groups, a yearly fecal exam is recommended.
Let’s talk about the specifics of these panels!
Fecal Exam-
This test requires approximately a golf ball sized amount of fresh stool. The sample looks for intestinal parasites such as hookworms, roundworms, whipworms, giardia, and coccidia. While most dogs are on monthly preventatives that should protect them from many of these parasites, not all are covered by routine prevention. For indoor only cats, a “community sample” is sufficient. In dogs it’s best to check a sample for each dog. The sample should be relatively fresh. A dry, several day old sample from the litterbox or the yard is not the most accurate sample to collect.
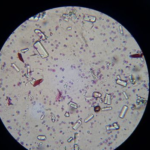
Urinalysis-
Sometimes this sample can be collected by what we call “free catch”- that is collected by the pet owner at home. In these cases the cleaner the better, and the fresher the better. A clean, dry container should be used to collect a midstream urine sample. 2-3 tablespoons is a sufficient quantity. In most cases, the best urine sample is a sterile sample, collected by a technique called cystocentesis. The vet or the CVT collects the sample by sterile needle directly from the bladder (usually with an ultrasound to guide the collection). When used as a screening tool, we usually are looking for changes in pH, protein, glucose, urine concentration, and crystals. This can tip us off to diseases such as diabetes, kidney disease, Cushing’s disease, Feline Idiopathic Cysitits, and bladder stones.
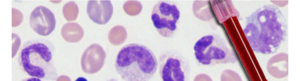
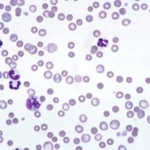
CBC-
Complete Blood Count. This test requires a blood draw, and to be placed into a blood collection tube that stops clotting. The CBC gives information on red blood cells, white blood cells, and platelets. This test can aid in diagnosing infection, inflammation, some types of cancer, medication reactions, and autoimmune disease.
Chemistry-
This test requires a blood draw and to be placed in a sample collection tube that is spun down to separate the red blood cells from the serum. Chemistry is a broad term, a number of different “panels” can be checked. A very basic panel generally has BUN and Creatinine (kidney values) and ALP and ALT (liver enzymes) and glucose. More detailed panels check electrolytes, albumin, globulin, total protein, phosphorus etc. This panel is used in diagnosis of many disease processes. Many changes (such as changes to kidneys and liver) can be caught on a chemistry panel before the patient is even showing any clinical symptoms of disease. Furthermore, pets who are on chronic medications (such as steroids, pain medications, behavioral modifying medications, and medications for allergies) should be doing routine screening.
Heartworm test-
A heartworm test requires a very small amount of blood. It does not require a separate blood draw from the Chemistry and CBC, but can be done independently. Heartworm disease is carried by mosquitoes. The immature heartworms develop into adult worms and live in the large vessels around the heart. Unfortunately affected dogs do not develop symptoms until the disease is already quite advanced. Treating heartworm disease is costly and invasive. Routine prevention is greatly preferred. Most heartworm preventative manufacturers will guarantee their product (that is pay for treatment!) if the pet has documented routine use of the product AND yearly heartworm tests. Unlike intestinal parasites, a fecal sample does not provide any information on heartworm disease.
Thyroid-
While dogs usually develop low thyroid (hypothyroidism) cats usually develop high thyroid (hyperthryoid). Dogs generally don’t need routine screening, but are instead tested for low thyroid hormone when their symptoms are suspicious for the disease. It is, however, recommended for senior cats to have screening for hyperthyroidism. Generally after 9 years of age we will start to recommend this routinely. If the thyroid hormone is high, treatment for hyperthyroidism can be started. Treatment is certainly more successful if we catch the change early and start treatment early!
FeLV/FIV testing-
Unique to cats, FeLV and FIV are viral infections. Transmission occurs by contact with other cats. Both diseases are retroviruses, which means they can cause infection without clinical signs. Infected cats can spread the disease to other cats, so it is recommended they be in single cat homes or homes with other positive cats. When symptoms do start to show, the diseases can be severe. Testing is only needed once for indoor only cats. Outdoor cats may need testing before being exposed to new cats, or if showing clinical signs of disease. Yearly/routine testing is generally not needed even for outdoor cats. Vaccination for feline leukemia is recommended for outdoor or indoor/outdoor cats, and testing should be done prior to starting the vaccine series.
If your head is spinning, fear not! The average pet owner only needs to know the following: your veterinary team is trained to make recommendations for both dogs and cats, and for all life stages. They are also happy to talk to you about the recommendations and about the specifics of your questions! These recommendations exist because we are scanning for diseases BEFORE clinical signs develop. In most cases we have greater success in managing a disease process the earlier it is caught!
We can learn a lot from a thorough history. That’s why when you bring your pet to the vet you will have to answer a lot of questions (sometimes more than once!). We can also learn a lot from a physical exam. Sometimes the physical exam is enough to give the answer! However, we can gain a LOT of information from running some lab work. Your vet may recommend bloodwork be performed when your pet is sick, as a screening prior to anesthesia, or just as part of a routine annual exam. Today we are going to focus on what we can learn from bloodwork performed as part of a routine annual exam!
Let me start by going through the recommendations that Highland Pet Hospital makes for each species and age group of pets.
Puppies (those under 1 year of age) have a recommendation of a fecal exam.
Adult dogs (1-7 years of age) have a recommendation of a heartworm test, yearly fecal exam, CBC, and abbreviated chemistry panel.
Senior dogs (8 years and up) are recommended to have a heartworm test, CBC, Chemistry (our default panel is a shortened panel, but in some cases a more thorough chemistry panel is indicated), and a urinalysis. A yearly fecal exam is also recommended.
Kittens (under 1 year of age) are recommended to have a FeLV/FIV test and a fecal test.
Young Adult Cats (1-2 years of age) are recommended to have a urinalysis and a yearly fecal test.
Adult Cats (4-8 years of age) are recommended to have a urinalysis, CBC, and abbreviated chemistry panel. A yearly fecal test is also recommended.
Senior Cats (9 years and up) are recommended to have a urinalysis, CBC, chemistry panel, and a Total T4. As with the other age groups, a yearly fecal exam is recommended.
Let’s talk about the specifics of these panels!
Fecal Exam-
This test requires approximately a golf ball sized amount of fresh stool. The sample looks for intestinal parasites such as hookworms, roundworms, whipworms, giardia, and coccidia. While most dogs are on monthly preventatives that should protect them from many of these parasites, not all are covered by routine prevention. For indoor only cats, a “community sample” is sufficient. In dogs it’s best to check a sample for each dog. The sample should be relatively fresh. A dry, several day old sample from the litterbox or the yard is not the most accurate sample to collect.
Urinalysis-
Sometimes this sample can be collected by what we call “free catch”- that is collected by the pet owner at home. In these cases the cleaner the better, and the fresher the better. A clean, dry container should be used to collect a midstream urine sample. 2-3 tablespoons is a sufficient quantity. In most cases, the best urine sample is a sterile sample, collected by a technique called cystocentesis. The vet or the CVT collects the sample by sterile needle directly from the bladder (usually with an ultrasound to guide the collection). When used as a screening tool, we usually are looking for changes in pH, protein, glucose, urine concentration, and crystals. This can tip us off to diseases such as diabetes, kidney disease, Cushing’s disease, Feline Idiopathic Cysitits, and bladder stones.
CBC-
Complete Blood Count. This test requires a blood draw, and to be placed into a blood collection tube that stops clotting. The CBC gives information on red blood cells, white blood cells, and platelets. This test can aid in diagnosing infection, inflammation, some types of cancer, medication reactions, and autoimmune disease.
Chemistry-
This test requires a blood draw and to be placed in a sample collection tube that is spun down to separate the red blood cells from the serum. Chemistry is a broad term, a number of different “panels” can be checked. A very basic panel generally has BUN and Creatinine (kidney values) and ALP and ALT (liver enzymes) and glucose. More detailed panels check electrolytes, albumin, globulin, total protein, phosphorus etc. This panel is used in diagnosis of many disease processes. Many changes (such as changes to kidneys and liver) can be caught on a chemistry panel before the patient is even showing any clinical symptoms of disease. Furthermore, pets who are on chronic medications (such as steroids, pain medications, behavioral modifying medications, and medications for allergies) should be doing routine screening.
Heartworm test-
A heartworm test requires a very small amount of blood. It does not require a separate blood draw from the Chemistry and CBC, but can be done independently. Heartworm disease is carried by mosquitoes. The immature heartworms develop into adult worms and live in the large vessels around the heart. Unfortunately affected dogs do not develop symptoms until the disease is already quite advanced. Treating heartworm disease is costly and invasive. Routine prevention is greatly preferred. Most heartworm preventative manufacturers will guarantee their product (that is pay for treatment!) if the pet has documented routine use of the product AND yearly heartworm tests. Unlike intestinal parasites, a fecal sample does not provide any information on heartworm disease.
Thyroid-
While dogs usually develop low thyroid (hypothyroidism) cats usually develop high thyroid (hyperthryoid). Dogs generally don’t need routine screening, but are instead tested for low thyroid hormone when their symptoms are suspicious for the disease. It is, however, recommended for senior cats to have screening for hyperthyroidism. Generally after 9 years of age we will start to recommend this routinely. If the thyroid hormone is high, treatment for hyperthyroidism can be started. Treatment is certainly more successful if we catch the change early and start treatment early!
FeLV/FIV testing-
Unique to cats, FeLV and FIV are viral infections. Transmission occurs by contact with other cats. Both diseases are retroviruses, which means they can cause infection without clinical signs. Infected cats can spread the disease to other cats, so it is recommended they be in single cat homes or homes with other positive cats. When symptoms do start to show, the diseases can be severe. Testing is only needed once for indoor only cats. Outdoor cats may need testing before being exposed to new cats, or if showing clinical signs of disease. Yearly/routine testing is generally not needed even for outdoor cats. Vaccination for feline leukemia is recommended for outdoor or indoor/outdoor cats, and testing should be done prior to starting the vaccine series.
If your head is spinning, fear not! The average pet owner only needs to know the following: your veterinary team is trained to make recommendations for both dogs and cats, and for all life stages. They are also happy to talk to you about the recommendations and about the specifics of your questions! These recommendations exist because we are scanning for diseases BEFORE clinical signs develop. In most cases we have greater success in managing a disease process the earlier it is caught!
Giardia. A little organism, a lot of trouble. Giardia is an intestinal parasite, but not a worm. It is a single celled organism called a Protozoa. Let’s learn some facts about this intestinal parasite which can be so tricky!
Lifecycle-
Giardia exists in two forms. The first is a hardy cyst, which can last in the environment for an extended period of time. Once consumed by a dog, the cyst becomes a trophozoite. This form attaches to the wall of the intestine to feed. The cysts are then shed in the feces and re-enter the environment.
Infection-
Dogs and cats are infected by consuming the cysts. This happens most commonly through ingestion of feces. Cysts can also be consumed by licking or sniffing the rear of an infected dog, or by consuming water infected with cysts. Dogs do seem to more frequently pick up the infection because they spend more time outside and are more prone to eat suspicious things than cats!
Symptoms-
Most commonly giardia causes diarrhea, occasionally with blood. Less commonly vomiting, weight loss, and changes in appetite are seen. The animals who are most susceptible to severe infection are very young puppies or kittens with high trophozoite burden, or immunocompromised dogs. Many animals, especially healthy adults, are completely asymptomatic!
Diagnosis-
A fecal sample is needed to diagnose giardia. The fecal sample is spun in a centrifuge with a fecal float solution, and the sample is examined under a microscope. Even so, it takes a practiced eye to see the very tiny cysts that are shed in the fecal sample. Occasionally an antigen test (looking for specific proteins on the giardia organism) is used to confirm a positive result. All of this testing has some limitations. Sometimes the organisms simply aren’t being shed when the fecal sample is checked. This is especially common in dogs with very small amount of trophozoites. If your dog has diarrhea, sometimes the veterinarian will recommend a second stool sample to be checked to ensure the sample is truly free of protozoal parasites. This is especially important for young animals.
Treatment-
Here’s where things get a little complicated. No “approved protocol” exists for giardia. That doesn’t mean we don’t know how to treat it! It just means there is a lot of minor variation between treatment protocols! This means individual veterinarians and veterinary clinics may simply choose different protocols. Most commonly Fenbendazole (Panacur) or metronidazole (Flagyl) are used. Often they are used together!
Prevention-
Cysts are immediately infectious, so picking up feces right away is helpful in preventing transmission. It is also recommended to wipe rear ends and paws after defecation. This prevents self reinfection, and reinfection of housemates. There is no preventative for giardia infection. While routine use of a heartworm preventative will protect your pet from many intestinal parasites, it will not protect against protozoal infections.
Rechecking-
Again, a great deal of variation exists in recommendations for when to recheck. Anywhere from 2-4 weeks is common. I generally like to recommend a 4-6 week recheck in an otherwise healthy patient. That gives the patient’s own immune system some time to kick in and help the infection along!
Can I get Giardia from my pet?-
Humans are susceptible to giardia infection, however, the most common way for humans to be infected is from contaminated water sources. The most common assemblage of the giardia organism is actually different between species. Humans are less susceptible to the canine assemblage, and there is virtually no cross contamination between cats and dogs. However, it’s still important to use good hygiene. Contamination from pets occurs through fecal oral contact- i.e. ingestion of the cysts from the fecal material. Wearing gloves to pick up feces and washing hands after handling feces prevents infection. This is especially concerning for high risk individuals- immunosuppressed, cancer patients, very young, and very old.
Is it true that it’s hard to get rid of Giardia?-
Tricky question. No, it’s actually pretty easy… most of the time. As a pretty common disease, we are constantly treating cases of giardia. Most show very mild (if any) symptoms, respond to the first round of treatment, and clear the infection. Occasionally a persistent infection does seem to develop. These persistent infections will remain (usually in decreasing numbers) through several rounds of treatments and rechecks. Often these patients are asymptomatic despite their persistent infection. Eventually we do get it cleared up. No pet ever keeps their giardia forever, some of them just seem to take longer to respond to the treatment protocol than others. It can be frustrating, but it does happen.
“He would never” (but he totally would!)
Things you think your dog would never do, but you never know.
This blog is inspired by my own dog, Jovi. A short time ago I was telling all of my coworkers about how our home is “grape and raisin” free. Our kids think grapes are a super special treat that they get to eat on vacation and at their friend’s houses. Last week I came home to find that Jovi had raided the baby sitter’s purse, and eaten most of her entire bag of raisin containing trail mix. I induced vomiting, and retrieved 14 raisins. She could never eat raisins, we don’t even have them in our house….. Except she totally did. Here’s a few “She would never” statements, and why they might not be as true as we want them to be!
“He’s great off leash, he would never run away from me”.
Even the best trained dogs can have unexpected things happen. A squirrel runs across the street, thunder booms and startles the pet, another dog is barking on the other side of the street. Unexpected scenarios can always pop up. If you are near a street, even if your dog is perfectly reliable, the best thing you can do to keep them safe is to keep them on a leash!
“She never eats anything silly”
I think the most ridiculous thing I’ve ever found inside a dog who “never eats anything” was an air pod earbud. Carpet is pretty common (it starts unraveling, and it just keeps unraveling). Feminine hygiene products and baby diapers are REALLY common. I actually think the addition of a baby to a home doubles the risk of ingestion of a non-food item by a dog who usually doesn’t eat anything. Diapers, bottle nipples, wipes, and toys are all really tempting treasures. Toddlers in the home makes the likelihood of ingesting grapes, raisins, chocolate, candy, and small toys triple! Guests in the home, or visiting a new environment (like the farm or a labor day cookout) also means “he never has access to anything” dogs might be exposed to something they normally wouldn’t have access to.
“He would never bite anyone”
I know I’m biased on this one. Lots of dogs who would “never bite” have tried to take a bite out of me! It’s not their fault, I’m pretty scary to an unsuspecting dog! Unfortunately, there are lots of reasons for even the best dogs to bite. Painful dogs are more likely to bite (for example, a dog who has been hit by a car is much more likely to bite when moved). Scared dogs are more likely to bite. Startled dogs are more likely to bite. A common scenario is a young kid falling on a sleeping dog. Sleeping dog is startled and bites the kid before thinking. All dogs will bite, some just have a higher threshold than others.
“She never goes outside, she can’t have fleas”
Fleas are sneaky. Limited outside time may minimize the risk of fleas, but it can’t eliminate the risk entirely. If your pup isn’t on a flea preventative, and starts itching, it’s always worth doing a thorough flea comb to make sure fleas haven’t taken up residence. I also recommend routine use of a flea and tick preventative, even for those who don’t go outside (especially if you live in a high traffic environment like an apartment or townhome!)
As a veterinarian, I absolutely have a biased perspective on these statements! However, I do think it’s responsible to acknowledge that nothing is 100%, and to take precautions to protect our dogs from the things we can protect them from, and to never make assumptions! We shouldn’t live in fear, but responsibility, planning, and thought is a good thing!
When in doubt, ask your veterinarian to help you plan the best care for your pup!
Vaccination Consternation?
Did you ever know you would be spending so much time thinking about infectious disease? As COVID-19 grips the world, many people are learning more about viruses and infectious disease than they ever wanted to know. While COVID-19 does not infect our pets, there are a number of infectious diseases that DO cause serious illness in our companion animals. Fortunately, many of the most devastating diseases have vaccines that help to keep our pets safe. It can be easy to get overwhelmed and lost in the vast number of recommendations for vaccines. Since most of us who work at vet clinics abbreviate the vaccines names, it can be hard to know the ABCs and LMNOPs of DAPP, DAP, Lepto, H3N2, and FVRCP.
Let me outline Highland Pet Hospital’s vaccine protocol for you.
Note that vaccine protocols will vary between clinics. This doesn’t mean one is right and one is wrong! Different geographic regions may have different recommendations, different pricing structures and doctor preference may alter how vaccines are given. This is ok, and means that the vets involved have given some thought to how best to keep your pet safe.
Dog vaccines at Highland are grouped into two categories.
First, Core Vaccines. Core Vaccines are Rabies and a combination vaccine called DAPP. A 1 year rabies is given to puppies, and repeated at the one year visit. At the two year visit, we start giving a 3 year rabies vaccine. The so called “DAPP” vaccine is for Distemper (a viral infection that affects respiratory tract and neurologic system), Adenovirus (a viral infection that affects the liver), Parainfluenza (a viral upper respiratory infection), and Parvo (a viral infection of the intestinal tract). After the first two years, the DAPP vaccine is separated out and rotates with the rabies vaccine so that dogs get Rabies, Parvo, and DAP in a three year rotation. In this way, we try to prevent over vaccination and allow for the greatest immune response to the vaccines. At Highland, all core vaccines are paid for with your annual wellness exam.
Second, a class of vaccines we call “social vaccines”. Social vaccines are evaluated based on the patient’s risk. Not all dogs will need to have these vaccines. The majority are needed by dogs who are in contact with other dogs, usually through boarding, grooming, or day care. These are bordetella (known more commonly as kennel cough) and CIV (or canine influenza virus). Bordetella and CIV cause upper respiratory signs, particularly coughing. The other vaccine we administer according to risk is called Leptospirosis (or lepto). This is a bacterial infection that is transmitted in urine. As such, dogs who are at risk are those in contact with water through hiking, runoff, streams, retention ponds, and garden ponds and those dogs who are in contact with wildlife. We do occasionally vaccinate for Lyme disease, but as Lyme disease is just one of the diseases carried by ticks, I tend to prefer a good flea and tick preventative protocol over vaccination for Lyme disease. Social vaccines are all included in a package that is purchased once yearly.
Cats are a little easier.
Core vaccines for cats are Rabies and a combination vaccine called FVRCP. We do try to be very careful with vaccine injections in cats, as cats are prone to a type of tumor that can develop at the injection site. Because of this, we select vaccines that do not have “adjuvent”. Adjuvent is included in some vaccines to enhance the body’s response to the vaccine, but cats’ bodies respond badly to adjuvant. Our rabies vaccine is non-adjuvented, and is given yearly. FVRCP stands for Feline Viral Rhinotracheitis, Calicivirus, and Panleukopenia. Rhinotracheitis is the feline herpes virus. Rhinotracheitis causes severe upper respiratory signs and ulceration of the cornea. Calicivirus causes upper respiratory signs as well, but the ulcerations are generally in the mouth. Panleukopenia is commonly referred to as feline distemper, and causes a variety of clinical signs. We have chosen an intranasal FVRCP vaccine, which is given into the nose to reduce the number of vaccine injections that need to be given to a cat. FVRCP is given every 3 weeks to kittens, repeated at 1 year, and then given every 3 years. The only elective vaccine for cats is a feline leukemia vaccine, which should be given to all cats who spend time outdoors. Feline leukemia is transmitted by exposure to cats who are carrying the disease. All feline vaccines are included in the cost of the annual exam.
Vaccines are extremely important to prevention of infectious disease. Rabies, though rare, is still seen in wildlife in the United States. Parvovirus is a deadly disease that is almost exclusively seen in dogs who have not been vaccinated. So, it is important to schedule an annual wellness visit with your veterinarian. At that visit you can discuss your pet’s lifestyle and determine which vaccines are most needed, and when they should be given.
Having a hard time getting your pet in for vaccines due to social distancing and quarantine? At Highland we will prioritize appointments and vaccine needs to the best of our ability. Sick pets come first. Pets needing rabies vaccines and puppies and kittens who have not yet been vaccinated will be our top priorities. Pets who are not due for rabies, and have previously had their core vaccines will not be considered priority during the quarantine period. This can seem scary, but never fear. Social distancing for people is also protecting our pets, as dogs and cats will not be boarding, grooming, or going to daycare during this time and thus not exposing themselves to infection. As restrictions on what is considered “essential” change, we will make every effort to have your pets seen promptly. During the quarantine period, our staff will always be available by phone and email to answer any questions you have! As a veterinarian, I feel constantly prepared to fight infectious disease! Join me in the war by vaccinating your pets, (and by washing your hands!)
Photobiomodulation
It’s like having coffee with your breakfast
If I say laser, what pictures immediately come to mind? Star trek weapons? Laser tag? The teacher’s red pointer? You may even conjure up a picture of laser surgery. What you probably didn’t picture is healing, tissue repair, decreasing inflammation, and increasing tissue perfusion. Did you know that laser therapy at an appropriate wavelength has a lot of uses in wound healing, pain management, and in treating inflammation?
Photobiomodulation is a fancy word for light therapy. Laser (which actually stands for light amplification by stimulated emission of radiation) is becoming increasingly popular to aid in healing and pain management! Here’s the secret: not all lasers are the same! At an appropriate wavelength, and used for an appropriate duration, laser therapy can be very therapeutic. (rather than destructive….)
Essentially photobiomodulation is a select wavelength of light that penetrates the tissue at a certain depth. It improves circulation, helps with pain management, causes vasodilation, improves muscle relaxation, and reduces inflammation at the cellular level. All of these things result in faster healing times, better pain control, and improved function.
How is the procedure performed?
The veterinarian prescribes a laser protocol, just as they would write a prescription for a medication. This prescription includes a location of the body and a duration of time. The laser can be administered by either a veterinary technician or by the veterinarian. The laser is positioned over the prescribed area. The laser is generally positioned lightly over a wound, or gently pressed into an area with soft tissue injury. This is not painful to the patient, and most pets receive the treatment very well. The hardest part is holding still! For some of our more wiggly patients, an aromatic snack is provided to improve the experience. One of our favorites is frozen baby food, right out of the jar. Where room temperature baby food can be quickly lapped up, frozen baby food provides a much longer distraction time!
Are there risks?
As with all procedures, there are risks. However, when the prescription is appropriate for the patient, these risks are really uncommon! When used correctly, side effects like thermal damage are very rare. The major safety risk is for both the people in the room, and the patient in the room. When the light from the laser enters the eye directly, retinal damage can occur. For this reason, anyone in the room where laser therapy is being performed will be asked to wear goggles. The patient gets to wear a pair of “doggles” during treatment. Let me be the first to say that doggles are significantly cuter than their human equivalent! Laser therapy is contraindicated in cancer patients, as the laser can make inappropriate cells (like cancer cells) grow faster too.
When do we recommend laser treatments?
Most commonly we use the laser on patients who need better pain control, or patients who need a lot of healing. Here’s a few examples:
- Wounds
- Fractures
- Post operative orthopedic patients- after an ACL repair or a bone fracture repair
- Arthritis
- ACL injuries (with or without surgery)
- Hip Dysplasia
- Back injury- Intervertebral Disc Disease
Laser is rarely the only therapy that is implemented. Rather laser therapy makes up a component of multimodal care. Multimodal care means implementing several methods of pain control and treatment. A classic example is a dachshund with back pain. Laser is an excellent addition to a balanced therapy with muscle relaxants, anti-inflammatory medications, and strict rest. You might say that laser therapy is the equivalent of adding coffee to your breakfast. Coffee alone doesn’t make for a good breakfast, but it makes the breakfast oh so much better!
If your pet is scheduled to undergo a major surgery, or if your pet struggles with pain from arthritis or injury, talk to your veterinarian about adding laser therapy as a part of his or her treatment!
© 2019 All Rights Reserved.